Nerve pain following a herniated disc is an all-too-common affliction that can drastically alter one's quality of life. This condition often manifests through persistent symptoms such as chronic pain, numbness, and muscle weakness, making everyday tasks a challenge. With millions of people experiencing herniated discs worldwide, understanding the subsequent nerve pain is crucial for effective management and relief.
understanding herniated discs and nerve pain
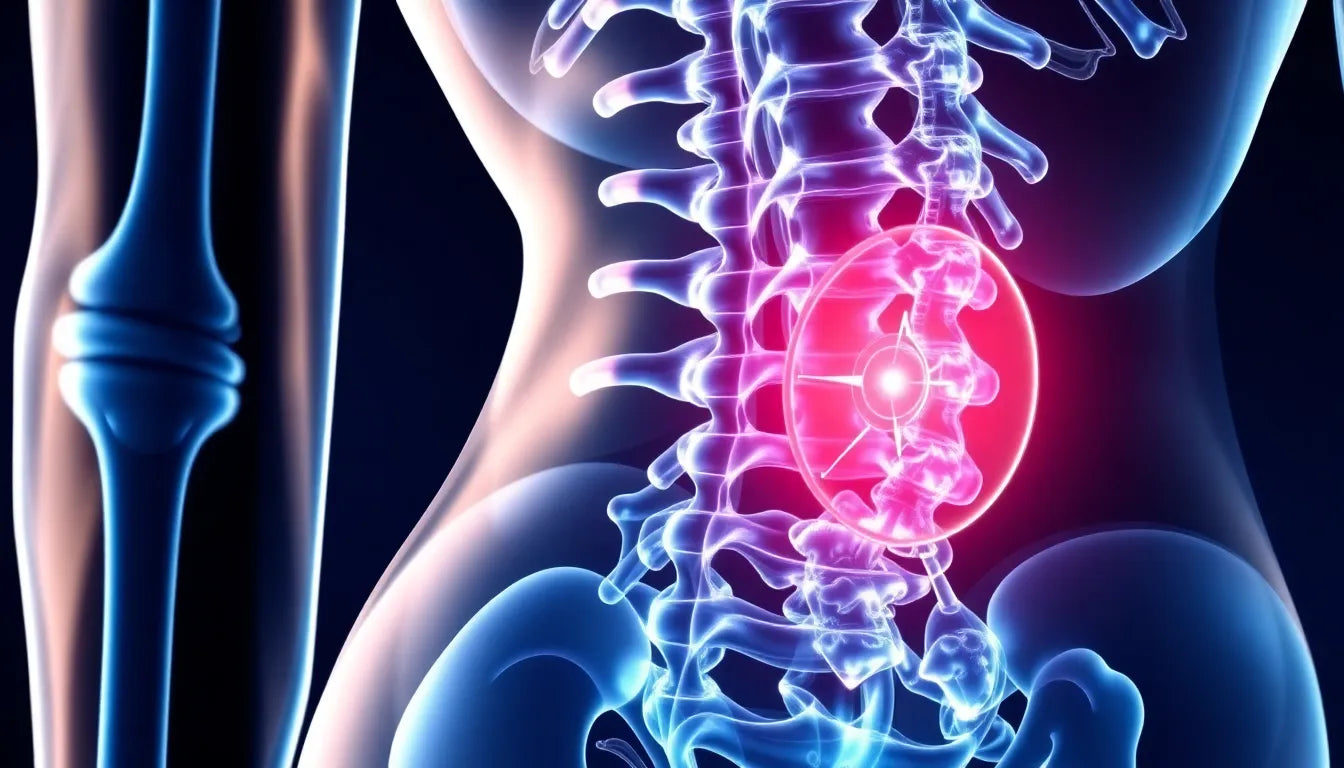
A herniated disc occurs when the soft, gel-like center of a spinal disc pushes through a crack in the tougher exterior casing. This protrusion can press on nearby nerves, leading to the pain and discomfort commonly associated with the condition. The severity of the symptoms varies depending on the location of the herniated disc and the extent of nerve involvement. For many, this nerve pain can become a debilitating issue, interfering with work, leisure, and even simple movements.
The pain resulting from a herniated disc is not just localized to the back. It can radiate to other parts of the body, causing a range of symptoms that can include sharp, shooting pains, tingling, or a burning sensation. These symptoms often follow the path of the affected nerve, which can lead to pain in the arms or legs, depending on the disc's location. Additionally, muscle weakness and a loss of reflexes can occur, further complicating the individual's ability to perform daily activities.
the importance of identifying symptoms and causes
Recognizing the symptoms and understanding the causes of nerve pain after a herniated disc is essential for managing the condition and seeking appropriate treatment. Early identification can prevent further nerve damage and improve recovery outcomes. By being aware of the potential signs, individuals can take proactive steps toward alleviating pain and improving their overall well-being.
This blog post aims to provide comprehensive information on the symptoms, causes, long-term effects, and treatment options for nerve pain following a herniated disc. By delving into these aspects, we hope to empower readers with the knowledge needed to address this condition effectively. In the sections that follow, we will explore the intricate details of the symptoms and mechanisms behind nerve pain, as well as the various treatment strategies available to help those affected find relief and regain control of their lives.
symptoms and effects of nerve pain after a herniated disc
Understanding the specific symptoms of nerve pain following a herniated disc is crucial for effective management and treatment. One of the most common symptoms associated with herniated discs in the lumbar region is sciatica. This condition occurs when the herniated disc presses on the sciatic nerve, leading to pain that radiates down the leg. Sciatica can cause significant discomfort and mobility issues, making it difficult for individuals to perform everyday activities.
Another prevalent symptom is numbness and tingling in the affected areas. This occurs when the compressed nerve disrupts normal sensory signals, resulting in a sensation often described as "pins and needles." Such sensations can be particularly distressing and may interfere with daily tasks. Additionally, muscle weakness and loss of reflexes are common, as the affected nerves are responsible for muscle control and coordination. These symptoms can severely impact an individual's ability to move and maintain balance.
| Disc Region | Symptom Location |
|---|---|
| Lumbar Herniated Disc | Legs and Feet |
| Cervical Herniated Disc | Arms and Shoulders |
causes and the mechanism behind nerve pain
The pain and discomfort experienced after a herniated disc are primarily due to the pressure exerted on nearby nerves. When the gel-like center of a disc protrudes through its outer layer, it can compress the nerves that run along the spine. This compression disrupts normal nerve function, leading to pain, numbness, and muscle weakness. The severity of these symptoms often depends on the extent of the nerve compression and the specific nerves affected.
Chronic pain development is a significant concern for individuals with herniated discs. Prolonged pressure on the nerves can lead to persistent pain that may not resolve even with treatment. This chronic pain can result in long-term nerve damage, making early intervention and management essential to prevent further complications.
In some cases, the body may attempt to heal the herniated disc by absorbing the protruding material. However, this process is not always successful, and the continued pressure on the nerves can lead to ongoing pain and discomfort. Understanding the underlying mechanisms of nerve pain after a herniated disc is vital for developing effective treatment strategies and improving patient outcomes.
By recognizing the symptoms and understanding the causes of nerve pain following a herniated disc, individuals can take proactive steps toward managing their condition. Early identification and intervention can prevent further nerve damage and improve recovery outcomes, allowing individuals to regain control of their lives and reduce the impact of this debilitating condition.
Long-term effects of nerve pain after a herniated disc
Understanding the potential long-term effects of nerve pain following a herniated disc is crucial for managing expectations and planning effective treatment strategies. One of the most concerning risks is the possibility of permanent nerve damage. Prolonged compression of nerves can lead to irreversible changes, resulting in persistent numbness or tingling sensations. In some cases, despite successful treatment of the herniated disc, the affected nerves may not fully recover, leaving individuals with lasting discomfort.
The impact on quality of life can be significant, as chronic nerve pain can hinder daily activities and reduce overall mobility. Tasks that were once simple, such as walking or lifting objects, may become challenging, affecting personal and professional life. Therefore, it is essential to address nerve pain promptly to mitigate these long-term effects and improve the individual's quality of life.
Treatment options and potential complications
When it comes to treating nerve pain after a herniated disc, a variety of options are available, ranging from conservative approaches to surgical interventions. Conservative treatments include rest, physical therapy, and medications aimed at reducing inflammation and alleviating pain. These methods are often the first line of defense and can be effective for many individuals in managing symptoms.
However, when conservative treatments do not provide sufficient relief, surgical interventions may be necessary. Surgery is typically considered when there is significant nerve compression leading to severe pain or neurological deficits. While surgical procedures can be successful in relieving pressure on the nerves, they come with potential risks and complications. These include the possibility of unsuccessful outcomes or the development of scar tissue, which can lead to persistent pain or recurrence of symptoms.
It is important for individuals to discuss the potential benefits and risks of each treatment option with their healthcare provider to make an informed decision. A personalized approach, taking into account the severity of symptoms and the individual's overall health, is essential for achieving the best possible outcomes.
Frequently Asked Questions
What are the early signs of nerve pain after a herniated disc?
Early signs include pain radiating along the affected nerve pathway, numbness, and tingling sensations. These symptoms often follow the path of the nerve affected by the herniated disc.
Can nerve pain from a herniated disc heal on its own?
In some cases, symptoms may improve with conservative treatments such as rest and physical therapy. However, severe cases might require surgical intervention to relieve nerve compression and alleviate pain.
How long does it take to recover from nerve pain after a herniated disc?
Recovery time varies depending on the severity of the nerve compression and the treatment approach. Some individuals may see improvement within weeks, while others may take months or require ongoing management for chronic symptoms.
What lifestyle changes can help manage nerve pain after a herniated disc?
Incorporating ergonomic aids, engaging in regular exercise, maintaining a healthy weight, and avoiding activities that strain the back can be beneficial in managing nerve pain. These lifestyle changes can help alleviate symptoms and prevent further complications.
By understanding the long-term effects, treatment options, and lifestyle adjustments, individuals can better manage nerve pain after a herniated disc and improve their overall quality of life. Early intervention and a comprehensive approach to treatment are key in finding relief and regaining control over daily activities.