Understanding the intricacies of spinal health is crucial, especially when it comes to conditions like herniated discs. A herniated disc, often referred to as a slipped or ruptured disc, occurs when the soft inner gel of a spinal disc pushes through its tougher exterior. This can lead to significant discomfort and impact your overall spinal health. The spine, being the central support structure of the body, plays a vital role in movement and flexibility, making it essential to maintain its integrity.
Early detection of a herniated disc is key to effective management and treatment. Recognizing the early-stage symptoms can prevent further deterioration and help avoid invasive treatments. By identifying these signs early, individuals can take proactive steps to manage their condition, potentially halting its progression. This blog post focuses on unveiling those early-stage herniated disc symptoms, empowering you with the knowledge to act swiftly and effectively.
Why early detection matters
The significance of early detection cannot be overstated. When caught in its initial stages, a herniated disc can be managed with less invasive methods, reducing the need for surgical intervention. Early identification allows for the implementation of lifestyle changes and therapeutic strategies that can alleviate symptoms and improve quality of life. Moreover, addressing the issue early can prevent the condition from escalating into more severe spinal problems that could require extensive treatment.
The primary focus of this post is to equip you with the ability to recognize early-stage symptoms of a herniated disc. These symptoms often include radiating pain, numbness, weakness, and tingling sensations. Understanding these signs is the first step in seeking the appropriate medical advice and intervention. By being informed, you can take control of your spinal health and ensure that any potential issues are addressed promptly.
Common symptoms of early-stage herniated disc
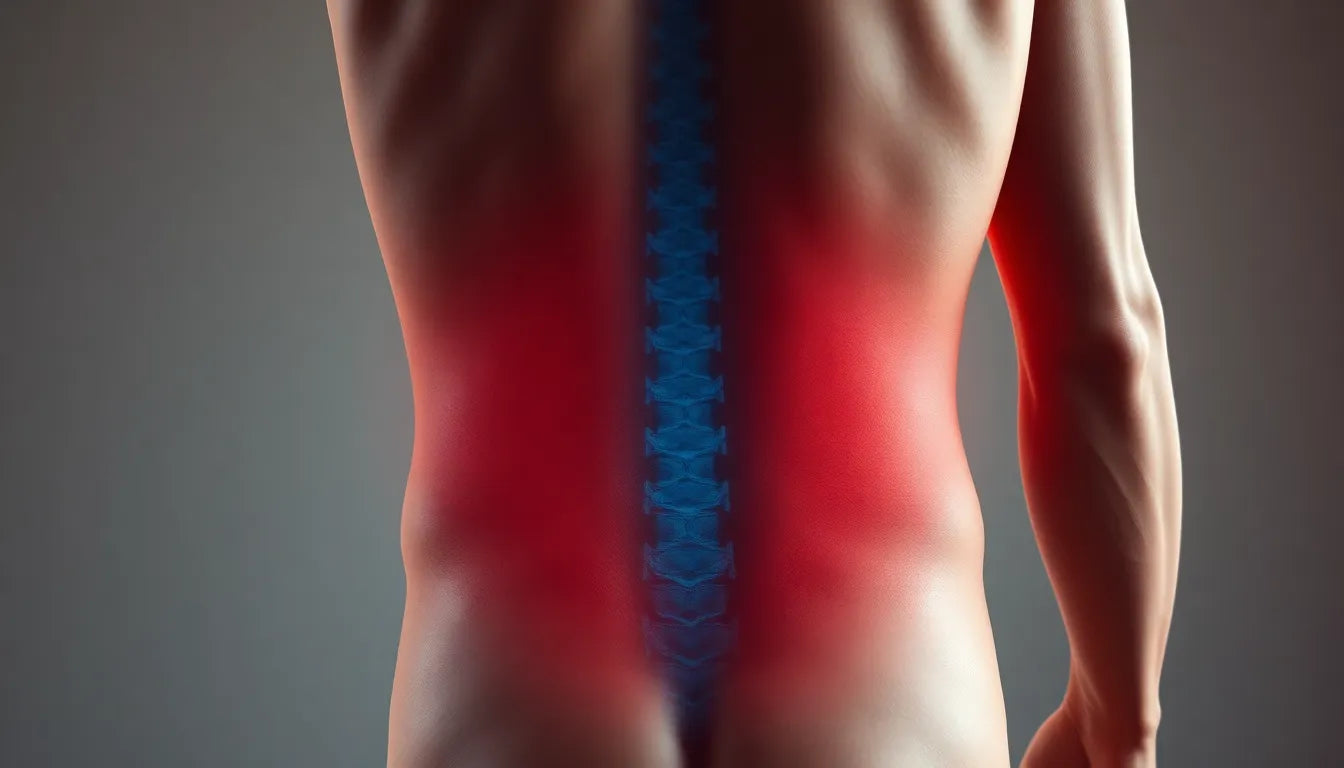
Recognizing the early symptoms of a herniated disc is crucial for timely intervention and management. One of the hallmark signs is radiating pain, which often stems from the lower back and travels down the legs. This pain is frequently associated with the sciatic nerve, leading to sensations that can be sharp, burning, or shooting. Such discomfort is not only distressing but can also hinder daily activities by limiting mobility and causing significant distress.
Another common symptom is numbness, weakness, and tingling. These sensations occur when the herniated disc compresses nearby nerves, affecting the arms or legs depending on the disc's location. This nerve compression can lead to a noticeable decline in muscle strength and coordination, impacting one's ability to perform routine tasks and diminishing overall quality of life. The presence of these symptoms often prompts individuals to seek medical advice due to the disruption they cause in daily functioning.
In addition to these generalized symptoms, individuals may experience localized pain. The specific location of the herniated disc determines where this pain is felt, whether it be in the lower back, neck, or chest. Understanding the site of pain is essential for accurate diagnosis and targeted treatment. This localized discomfort can vary in intensity and may be exacerbated by certain movements or postures.
It's also important to note the impact of pain during activities. Simple actions such as sitting, walking, or even sleeping can intensify the pain associated with a herniated disc. The discomfort during these activities is often a key indicator of the condition, as it suggests that specific movements or positions are aggravating the affected area. Recognizing these patterns can aid in developing a personalized approach to managing symptoms effectively.
Diagnostic approaches for early-stage herniated disc
Diagnosing a herniated disc in its early stages involves a combination of physical examinations and imaging tests. During a physical examination, healthcare professionals employ various tests to assess nerve function and pinpoint the source of pain. Techniques such as the straight leg raise, gait monitoring, and neurological checks are commonly used. These tests help determine the extent of nerve compression and guide the diagnostic process by highlighting areas of concern.
In addition to physical assessments, imaging tests play a crucial role in confirming the diagnosis of a herniated disc. Magnetic Resonance Imaging (MRI) is particularly valuable as it provides detailed images of the spinal cord and nerve roots, allowing for precise identification of the herniated disc's location and severity. Computed Tomography (CT) scans and X-rays may also be utilized to gain further insights into the spinal structure and any underlying issues. These imaging techniques are instrumental in formulating a comprehensive treatment plan tailored to the individual's needs.
Understanding these diagnostic approaches is vital for anyone experiencing early-stage herniated disc symptoms. Prompt and accurate diagnosis enables the initiation of appropriate interventions, which can significantly improve outcomes and prevent the condition from worsening. By being informed about the symptoms and diagnostic methods, individuals can take proactive steps toward managing their spinal health effectively.
Causes and risk factors of early-stage herniated disc
Understanding the causes and risk factors associated with early-stage herniated disc symptoms is essential for prevention and management. One of the primary contributors is age-related wear and tear. As we age, the spinal discs naturally lose some of their water content, leading to decreased flexibility and increased susceptibility to tears and ruptures. This degeneration can significantly heighten the risk of developing a herniated disc.
Physical demands also play a crucial role in herniated disc development. Occupations or activities that involve heavy lifting, repetitive movements, or sudden spinal twists can place undue stress on the spine. Over time, these physical demands can lead to disc herniation, especially if proper lifting techniques and posture are not maintained.
Another significant factor is weight. Carrying excess weight puts additional stress on the spine, particularly the lower back, increasing the likelihood of disc herniation. Maintaining a healthy weight through diet and exercise can reduce this risk and promote overall spinal health.
Preventive and treatment perspectives
Adopting preventive measures and understanding treatment options are vital in managing early-stage herniated disc symptoms. Lifestyle adjustments are fundamental in prevention. Incorporating ergonomic practices in daily activities, such as maintaining good posture and using proper techniques when lifting objects, can significantly lower the risk of disc herniation. Additionally, regular exercise and weight management are crucial for strengthening the back muscles and reducing spinal stress.
When it comes to treatment options, conservative therapies are often the first line of defense. Physical therapy can be highly effective in strengthening the muscles around the spine, improving flexibility, and alleviating pain. Medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help manage pain and reduce inflammation. In more severe cases, where conservative methods do not provide relief, more intensive treatments like epidural steroid injections or surgery might be considered.
Frequently Asked Questions
What are the first signs of a herniated disc?
The initial signs of a herniated disc often include mild pain or tingling sensations in the affected area. Over time, these symptoms can progress to more pronounced pain, numbness, or weakness, particularly if a nerve is compressed.
Can a herniated disc heal on its own?
In many cases, a herniated disc can heal naturally over time, especially with appropriate rest and conservative treatment. Factors such as the severity of the herniation, age, and overall health can influence the recovery process.
When should I see a doctor for back pain?
If back pain persists for more than a few weeks, is severe, or is accompanied by symptoms like numbness, weakness, or difficulty controlling bladder or bowel functions, it is crucial to seek medical evaluation promptly.
How is a herniated disc diagnosed?
Diagnosis typically involves a combination of physical examinations and imaging tests. Physical exams assess nerve function and pain source, while imaging tests like MRI and CT scans provide detailed views of the spine to confirm the diagnosis.
What lifestyle changes can help prevent a herniated disc?
To reduce the risk of herniated discs, it is important to maintain a healthy weight, practice proper lifting techniques, and engage in regular exercise to strengthen the back and core muscles. Additionally, ensuring ergonomic work and living environments can help protect the spine from excessive strain.
Sources
- Jenkins, T. (2023). "Herniated Disc Symptoms." Jenkins NeuroSpine.
- UCHealth. (2023). "Herniated Disc Overview and Diagnosis."
- International Spine, Pain & Performance Center. (2023). "Herniated Disc: Causes and Treatment."
- WebMD. (2023). "Herniated Disc Symptoms and Diagnosis."
- New York City Spine. (2023). "Symptoms and Treatment of Herniated Discs."