Back pain is a common ailment that affects millions of people worldwide, often disrupting daily routines and diminishing quality of life. Among the various causes of back pain, herniated discs are frequently identified as a primary culprit. Understanding where it hurts when you have a herniated disc is crucial for effective management and relief of symptoms.
Understanding a herniated disc
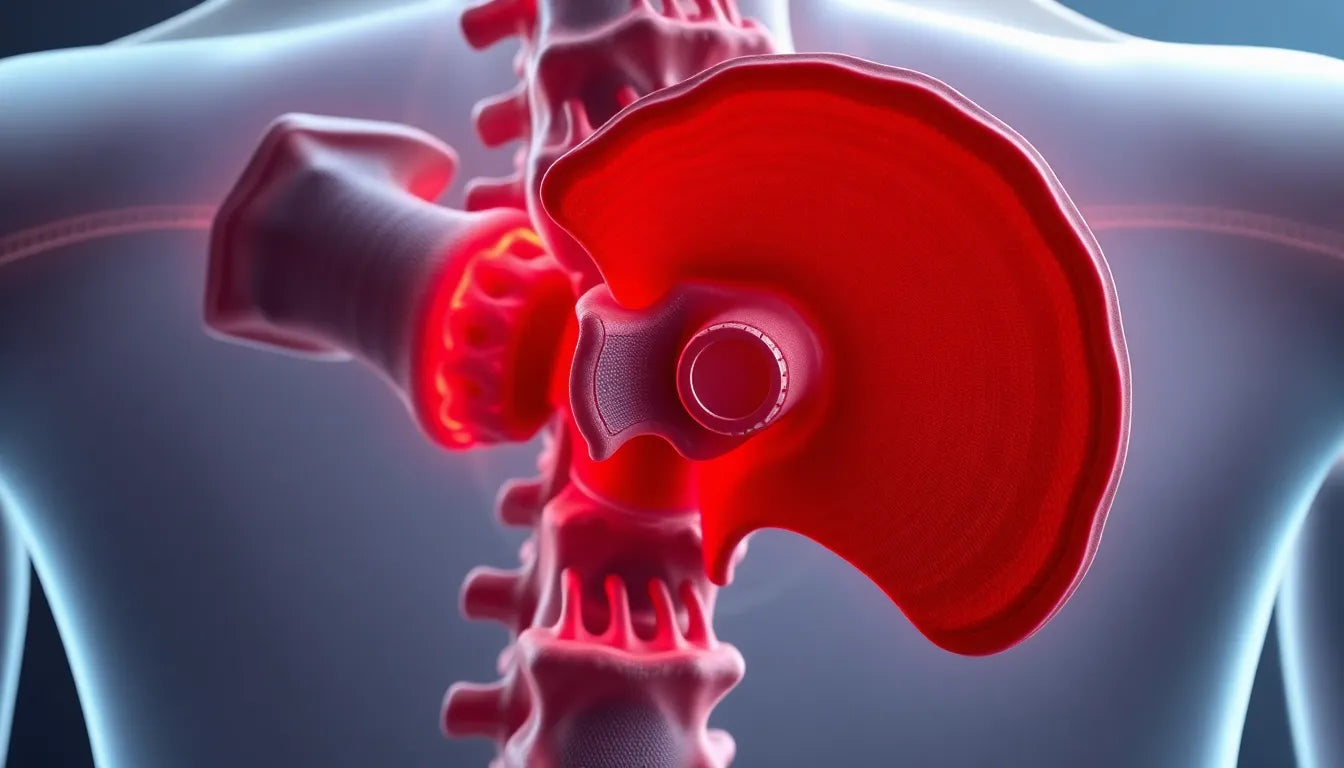
A herniated disc occurs when the soft inner gel of a spinal disc protrudes through a tear in its tougher exterior. This condition can lead to irritation of nearby nerves, resulting in pain, numbness, or weakness in an arm or leg. The spine, composed of vertebrae cushioned by discs, plays a vital role in supporting body movement and flexibility. When a disc herniates, it can disrupt this balance, causing discomfort and limiting mobility.
Typically, herniated discs are most common in the lower back (lumbar spine), but they can also occur in the neck (cervical spine). The location of the herniation determines where the pain is felt, making it essential to identify the specific areas affected to tailor treatment effectively.
Purpose of this post
This blog post aims to explore the typical pain locations associated with herniated discs, providing a comprehensive overview for those experiencing symptoms or seeking information. By understanding where it hurts, individuals can better communicate their symptoms to healthcare providers and pursue appropriate interventions. Whether you're dealing with a new diagnosis or have been managing a herniated disc for some time, this guide will help you navigate the complexities of this condition.
Symptoms and pain locations of a herniated disc
When a herniated disc occurs, the pain is often not confined to the back itself but can radiate to other areas. The most common pain distribution involves the buttocks, the back of the thigh, and extending into the calf. This pattern is commonly referred to as sciatica, a condition where the sciatic nerve is affected, leading to pain that can be both sharp and burning. This discomfort is typically more pronounced when engaging in activities such as coughing, sneezing, sitting for prolonged periods, driving, or bending forward.
Visualizing the affected areas can be beneficial for understanding the scope of pain. Imagine a diagram of the spine where the lower back, specifically the lumbar region, is highlighted. From there, lines extend down through the buttocks and along the back of the leg, illustrating the typical path of pain experienced by those with a herniated disc.
Common locations of herniation in the spine
The lumbar spine is the most frequent site for disc herniation, particularly between the L4-L5 and L5-S1 levels. These segments are highly susceptible due to their critical role in supporting the weight of the upper body and facilitating a wide range of movements. The stress placed on these discs during everyday activities makes them prone to wear and tear, increasing the likelihood of herniation.
In addition to pain, individuals with a herniated disc may experience a variety of other symptoms. Numbness and tingling sensations are common, often manifesting in the legs or feet. Muscle spasms and leg cramps can also occur, contributing to discomfort and mobility challenges. In more severe cases, individuals might experience leg weakness or even foot drop, a condition where lifting the front part of the foot becomes difficult, potentially leading to tripping or difficulty walking.
Additional symptoms and their implications
Understanding the full range of symptoms associated with a herniated disc is crucial for effective diagnosis and treatment. Besides the primary pain locations, recognizing additional signs such as numbness, tingling, and muscle weakness can help in assessing the severity of the condition. These symptoms arise due to the pressure exerted on the nerves by the herniated disc, disrupting normal nerve function.
For those experiencing these symptoms, it is essential to consider seeking medical advice. Early intervention can prevent further deterioration and aid in developing a comprehensive treatment plan. Such a plan might include physical therapy, medication, or in some cases, surgical intervention to relieve pressure on the nerves and restore function.
In conclusion, understanding where it hurts when you have a herniated disc is a critical step in managing the condition. By identifying the typical pain distribution and accompanying symptoms, individuals can better communicate their experiences to healthcare providers, paving the way for effective treatment and improved quality of life. As we continue to explore the impact of herniated discs, it becomes clear that knowledge and awareness are key components in navigating this common yet challenging condition.
Impact of a herniated disc on daily life
Living with a herniated disc can significantly affect one's quality of life. The persistent pain and discomfort often interfere with daily activities, making simple tasks like sitting, walking, or even sleeping challenging. Many individuals find that their ability to engage in physical activities is limited, which can lead to a decrease in overall fitness and well-being. Understanding the symptoms and their impact is crucial for managing the condition effectively and maintaining a good quality of life.
Moreover, the emotional toll of dealing with chronic pain should not be underestimated. Anxiety and depression can arise from the stress of managing a herniated disc, highlighting the importance of a holistic approach to treatment that addresses both physical and mental health.
Treatment options for herniated discs
When it comes to treating a herniated disc, options range from conservative approaches to surgical interventions. Initially, most healthcare providers recommend non-surgical treatments, such as physical therapy, which can help strengthen the muscles around the spine and alleviate pressure on the affected disc. Pain management techniques, including medications and epidural steroid injections, may also be prescribed to reduce inflammation and discomfort.
In cases where conservative treatments do not provide sufficient relief, surgical options might be considered. Procedures such as discectomy or laminectomy aim to remove or relieve pressure from the herniated portion of the disc. It is essential for individuals to discuss the potential risks and benefits of each treatment option with their healthcare provider to determine the best course of action.
Ergonomic aids, such as supportive chairs and mattresses, can also play a vital role in managing symptoms. These aids help maintain proper posture and reduce strain on the spine, contributing to pain relief and preventing further injury.
Frequently asked questions
What are the symptoms of a herniated disc?
The primary symptoms of a herniated disc include pain, numbness, and muscle weakness. Pain often radiates from the back to the buttocks, thighs, and calves, a condition known as sciatica. Numbness and tingling may occur in the legs or feet, and in severe cases, individuals may experience muscle weakness or difficulty lifting the foot, known as foot drop.
How is a herniated disc diagnosed?
A herniated disc is typically diagnosed through a combination of physical examinations and imaging tests. A healthcare provider will assess the patient's symptoms and may order an MRI or CT scan to visualize the affected area and confirm the diagnosis.
Can a herniated disc heal on its own?
In many cases, a herniated disc can improve over time with rest and conservative treatment. The body can reabsorb the herniated material, reducing pressure on the nerves. However, if symptoms persist or worsen, medical intervention may be necessary.
What are the treatment options for a herniated disc?
Treatment options for a herniated disc include non-surgical approaches such as physical therapy, pain medications, and lifestyle modifications, as well as surgical interventions like discectomy or laminectomy. The choice of treatment depends on the severity of the symptoms and the individual's overall health.
How can ergonomic aids help with a herniated disc?
Ergonomic aids, such as specially designed chairs, mattresses, and lumbar supports, can help maintain proper posture and reduce strain on the spine. These aids play a crucial role in alleviating pain and preventing further injury, making them a valuable component of a comprehensive treatment plan for a herniated disc.